When a pharmaceutical giant sues a telehealth company over weight-loss drugs, it sounds like the beginning of a streaming documentary.
But this isn’t Netflix. It’s healthcare, and it’s messy, important, and a little hilarious if you’ve been in this space long enough to appreciate the chaos.
The recent lawsuit filed by Novo Nordisk against Hims & Hers is about much more than corporate drama. It sits at the crossroads of three very real issues:
- Patient safety,
- Medication affordability
- The future of GLP-1 access for obesity and diabetes
So is this lawsuit a positive step forward — or a step backward?
As with most things in healthcare, the answer is: yes. (Clear as mud.)
What’s Happening?
Novo Nordisk, the maker of Wegovy and Ozempic (semaglutide), filed a federal lawsuit alleging that Hims & Hers was selling compounded versions of its GLP-1 medications that violate patent protections and fall outside FDA approval standards.
Hims & Hers had been marketing lower-cost compounded semaglutide options — including pill formulations — at prices dramatically lower than the brand-name injectables.
Novo argues that these compounded products are not FDA-approved, that they may vary in potency or formulation, and that their sale infringes on intellectual property Hims & Hers has since pulled certain offerings amid regulatory pressure.
Translation: The GLP-1 boom just got a courtroom subplot.
Why “This Is a Good Thing”
1. Safety Isn’t Optional (Boring yes, optional no.)
Let’s start with what shouldn’t be controversial.
GLP-1 medications are powerful metabolic therapies. They influence glucose regulation, appetite signaling, gastric emptying, and cardiovascular risk. They are not “just weight loss shots.” They are not smoothie add-ins.
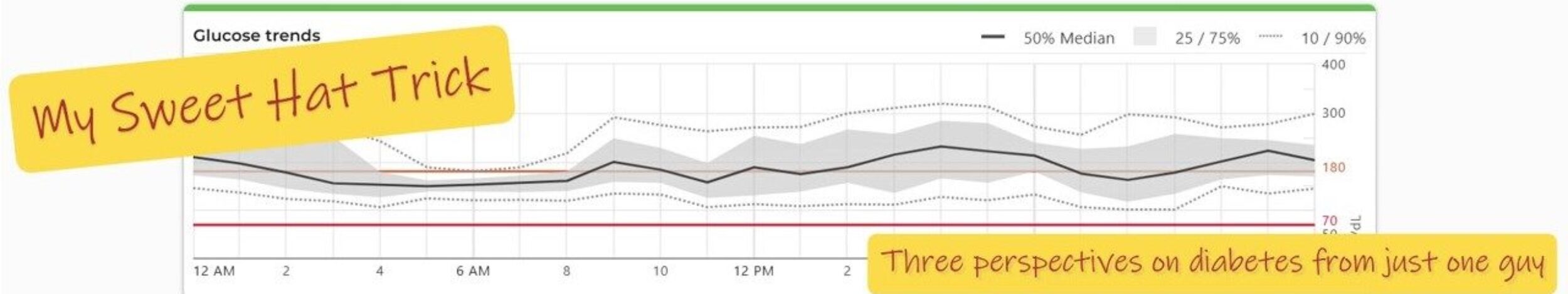
In diabetes care, dosing precision matters. A small difference in formulation can mean:
- More nausea
- Less efficacy
- Glucose instability
- Or unexpected side effects
FDA-approved medications go through:
- Rigorous clinical trials
- Manufacturing oversight
- Stability testing
- Ongoing safety monitoring

A helpful analogy is baking a cake.
If you taste an incredible cake and decide to recreate it, knowing it contains flour, eggs, sugar, oil, and milk is a start. But without the exact measurements, mixing process, temperature, and bake time, you’re guessing.
It might look similar.
It might even taste decent.
But it won’t be identical.
Medications are no different.
Two products can contain the same active ingredient — like semaglutide — but differ in concentration, purity, stability, or absorption. In chronic disease management, those differences matter.
Compounded medications absolutely have an important role in healthcare — particularly during shortages or when patients need customized formulations. But they do not go through the same FDA approval pathway as branded products.
If the concern is inconsistent dosing or quality variation, that isn’t corporate nitpicking.
That’s clinical reality.
From a safety perspective, reinforcing regulatory guardrails is not unreasonable — especially when we’re talking about medications people may take for years.
2. Innovation Isn’t Free
Here’s the less popular but still relevant point: drug development is expensive.
Bringing a medication to market takes years of research, failed attempts, clinical trials, and regulatory review. Patent protections are part of how companies recoup that investment and fund future innovation.
Without patents, we likely wouldn’t have GLP-1 therapies at all.
Now — whether pricing models are appropriate is an entirely separate (and passionate) discussion. But protecting intellectual property is consistent with how the current system operates.
In other words: Novo didn’t suddenly invent capitalism last Tuesday.
Why “This Is a Problem”
Now we pivot. Because the other side of this conversation is just as real.
1. Access Is the Elephant in the Room
GLP-1 medications have been transformative: they lower A1C, support meaningful weight loss, reduce cardiovascular risk, and improve quality of life.

Lower A1C.
Meaningful weight loss.
Reduced cardiovascular risk.
Improved quality of life.
But they also come with a price tag that can make insurance deductibles weep softly in the corner.
Coverage for obesity treatment remains inconsistent. Many plans exclude it entirely. Out-of-pocket costs can rival a car payment.
When patients can’t access approved medications due to cost, they look for alternatives.
Not because they’re reckless. Not because they’re trying to game the system. Because they want treatment.
Hims & Hers marketed compounded semaglutide at a fraction of brand-name prices. For some patients, that wasn’t about convenience — it was about finally being able to participate in modern metabolic care.
If those lower-cost options disappear without broader affordability solutions, the access gap widens again.
And metabolic disease does not pause politely while legal arguments unfold.
2. The System Created This Tension
Compounded GLP-1 products gained traction during drug shortages, when demand dramatically outpaced supply.

Now, demand is high, prices are high, and people are looking for ways to participate in modern metabolic care. It’s a classic case of supply, demand, and reality bumping heads with regulation.
The lawsuit isn’t just about who’s right or wrong — it’s about how complex healthcare delivery really is and highlights a deeper systemic issue:
We have breakthrough science. We have demand. We have outcomes data. But we do not have universal affordability. And until that changes, the friction between pharma, telehealth, compounding pharmacies, regulators, insurers, and patients will continue.
(Healthcare really does know how to keep things interesting. Maybe this should be on Netflix.)
So Is This Good or Bad?
It depends on your lens:
- From a safety lens, reinforcing FDA oversight and manufacturing consistency is positive.
- From an access lens, restricting lower-cost alternatives without addressing affordability is problematic.
- From a patient lens, it feels frustrating that life-changing therapies can be both revolutionary and financially out of reach.
The Real Question
Why are so many patients turning to compounded alternatives in the first place?
If FDA-approved medications were broadly accessible and affordable, the demand for copycat versions would shrink dramatically.
Patients don’t wake up hoping to bypass regulatory systems. They wake up wanting:
- Stable blood sugars
- Sustainable weight management
- Reduced health risks
- A plan they can actually afford
That shouldn’t feel radical.
My Perspective
As someone who works in diabetes care, I believe two things can be true at the same time:
Patients deserve medications that are safe, consistent, and evidence-based. AND Patients deserve affordable access to those medications.
This lawsuit may reinforce safety standards. But unless it is paired with meaningful movement on pricing and insurance coverage, it risks being perceived as protection of profits rather than protection of patients.
The future of obesity and diabetes care shouldn’t be determined solely in courtrooms.It should be shaped by policies that make breakthrough therapies both safe and accessible — without requiring patients to choose between innovation and affordability.
Because metabolic health is complicated enough. The access to treat it shouldn’t be.